More Information
Submitted: March 16, 2023 | Approved: March 30, 2023 | Published: March 31, 2023
How to cite this article: Marcos PA, Fuentes EG, Monrobe MM, Picón MOA, Mª del Rocío MT, et al. Management and use of vacuum systems in a surgery ward. Clin J Nurs Care Pract. 2023; 7: 006-008.
DOI: 10.29328/journal.cjncp.1001045
Copyright License: © 2023 Marcos PA, et al. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Management and use of vacuum systems in a surgery ward
Pilar Aragundez Marcos, Eugenia Gómez Fuentes, Manuela Moreno Monrobe, María Oliva Artilllo Picón, Mª del Rocío Mendoza Talaverón, Inés Mª Fernández Luque, Rosa M Jimenez-Rodriguez* and Francisco Javier Padillo Ruiz
Department of Surgery, Virgen del Rocío University Hospital, Seville, Spain
*Address for Correspondence: Rosa M Jimenez-Rodriguez, Department of Surgery, Virgen del Rocío University Hospital, Seville, Spain, Email: [email protected]
Vacuum therapy has become a new option in the treatment of wounds in surgery. More recently this therapy has also been used as a treatment for anastomotic leakages in association or not to emergency surgery. The management of these devices should be familiar to all the staff in a surgical ward.
Wound infections are one of the most common complications in surgery [1]. The treatment starts with antibiotics but also good care of the wound is needed. Several types of management have been described but in the last few years, vacuum therapy has become a popular option [2].
This vacuum therapy has also been used for wall dehiscence, pilonidal sinus disease, and a variety of conditions [3-5]. In the last few years, this therapy has been used for the treatment of anastomotic colorectal leakages with success ranging from 75% to 100% regarding the author [6].
The aim of the present work is to review the management of vacuum therapy in a surgical ward.
Vacuum therapy for infected wounds
In a sterilized setting, the wound should be cleaned and measured carefully. The sponge should be measured and divided accordingly to the size of the wound. In our experience, the size of the sponge should be at least 1 cm smaller in its diameter than the wound allowing the wound to approach the sponge decreasing the size of the defect with every change. Once the sponge is placed and the borders of the wound adjusted, a drape should be placed on top. To favor the adhesion of the drape, the borders of the wound should be dried. A small hole is done at this point in the drape in the place where the sponge is bigger to stick the drape with the tube that would be connected to the suction pump. We recommend keeping a -100 mm Hg negative pressure.
Vacuum therapy for anastomotic leakages
The technique was already published by Jimenez-Rodriguez, et al. [7]. In a summary, VAC is a technique that consists of the insertion of an open-cell polyurethane foam sponge into the wound (B. Braun Medical BV, Melsungen, Germany). The wound is irrigated with a normal saline solution and the sponge dressing is cut according to the size and geometry of the leak and the corresponding cavity. Two or more sponges are used whenever the wound size is too large for a single dressing. A gastroscope is then placed into the deepest point of the cavity and is connected to an introducer tube. The gastroscope is removed, and the sponge moistened with lubricant is pushed through the tube and finally released at the far end of the cavity. The plastic tube is then withdrawn. Finally, the correct position of the device is monitored, and the sponge is connected to a suction pump (Redyron® PLUS TRANS suction device, Melsungen, Germany) (Figures 1,2).
Figure 1: Image showing one vacuum device while in use by a patient.
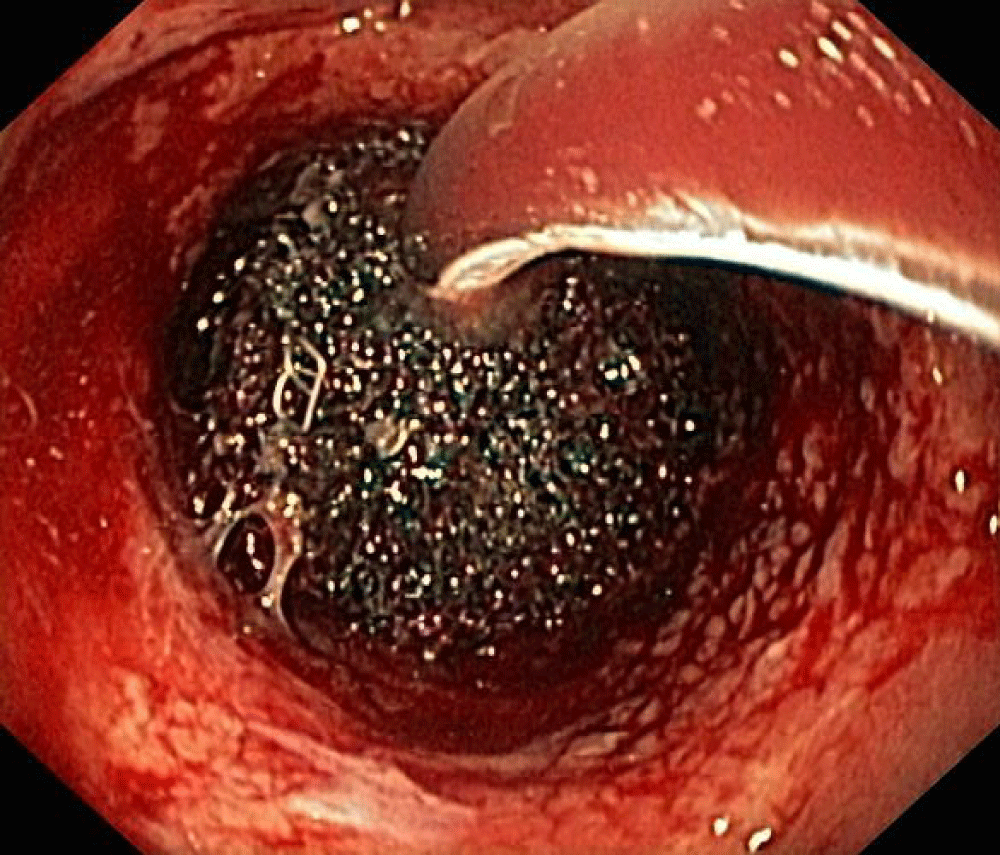
Figure 2: Sponge under used in a colorectal leak.
This suction pump is the device we should watch once the patient is in the ward. It delivers a constant level 2 negative pressure (375 mm hg). The sponge is kept in place by the suction effect in the cavity, and no drapes or other devices are needed to secure the system. Level 2 pressure is used initially for greater aspiration, since there is usually more necrotic material, in the first replacement we modify it to Level 1 (150 mm hg).
The sponge system is changed every 3-5 days to avoid the adherence of granulation tissue, which may result in painful removal.
The benefits of negative pressure have been demonstrated [3-5,7]. The attraction of cells and the suction of fluids have been some of the advantages of this therapy. Faster healing of would and recovery of patients with shorter stays support its use [8,9].
Vacuum therapy has been proven to be useful in the treatment of infected wounds and anastomotic leakages [8,9]. In both situations, the staff in the ward should be aware of the care needed by these patients. The technique can be used in a hospital setting or an ambulatory setting [10]. Independently of the location of the patient and in case of failure of the therapy, a leak in the pump or a defect of the sealing drape should be considered.
This vacuum therapy is a common device that should be known by the staff in a surgical ward due to its popular use. Due to the differences between health care systems and hospitals, not all are managed by surgeons, sometimes these devices are managed only by surgeons. But even though, all staff should know how to deal with a possible leak in the drape or other signs of alarm. This is one of the limitations of this paper because not all centers allow non-MD staff to manage these devices. Also, the cost is a limitation because not all hospitals have these therapies and even when it is available, sometimes is restrictive due to the price.
Nevertheless, current trends show earlier discharge of our patients and the use of vacuum therapy in ambulatory settings could be the key to avoiding extra cost and to be the ideal situation in the management by home-visiting nurses.
In this work, we reviewed some of the technical aspects of this therapy that should be known in a surgery ward.
Vacuum therapy is a common device in a surgical ward and it should be known by the staff. It could be used in the treatment of open wounds or colorectal leakages.
- Reeves BC, Rooshenas L, Macefield RC, Woodward M, Welton NJ, Waterhouse BR, Torrance AD, Strong S, Siassakos D, Seligman W, Rogers CA, Rickard L, Pullyblank A, Pope C, Pinkney TD, Pathak S, Owais A, O'Callaghan J, O'Brien S, Nepogodiev D, Nadi K, Murkin CE, Munder T, Milne T, Messenger D, McMullan CM, Mathers JM, Mason M, Marshall M, Lovegrove R, Longman RJ, Lloyd J, Lim J, Lee K, Korwar V, Hughes D, Hill G, Harris R, Hamdan M, Brown HG, Gooberman-Hill R, Glasbey J, Fryer C, Ellis L, Elliott D, Dumville JC, Draycott T, Donovan JL, Cotton D, Coast J, Clout M, Calvert MJ, Byrne BE, Brown OD, Blencowe NS, Bera KD, Bennett J, Bamford R, Bakhbakhi D, Atif M, Ashton K, Armstrong E, Andronis L, Ananthavarathan P, Blazeby JM. Three wound-dressing strategies to reduce surgical site infection after abdominal surgery: the Bluebelle feasibility study and pilot RCT. Health Technol Assess. 2019 Aug;23(39):1-166. doi: 10.3310/hta23390. PMID: 31392958; PMCID: PMC6698727.
- Banwell PE, Musgrave M. Topical negative pressure therapy: mechanisms and indications. Int Wound J. 2004 Jun;1(2):95-106. doi: 10.1111/j.1742-4801.2004.00031.x. PMID: 16722882; PMCID: PMC7951556.
- Pliakos I, Papavramidis TS, Michalopoulos N, Deligiannidis N, Kesisoglou I, Sapalidis K, Papavramidis S. The value of vacuum-assisted closure in septic patients treated with laparostomy. Am Surg. 2012 Sep;78(9):957-61. PMID: 22964204.
- McGuinness JG, Winter DC, O'Connell PR. Vacuum-assisted closure of a complex pilonidal sinus. Dis Colon Rectum. 2003 Feb;46(2):274-6. doi: 10.1007/s10350-004-6535-z. PMID: 12576904.
- Perathoner A, Klaus A, Mühlmann G, Oberwalder M, Margreiter R, Kafka-Ritsch R. Damage control with abdominal vacuum therapy (VAC) to manage perforated diverticulitis with advanced generalized peritonitis--a proof of concept. Int J Colorectal Dis. 2010 Jun;25(6):767-74. doi: 10.1007/s00384-010-0887-8. Epub 2010 Feb 11. PMID: 20148255.
- Weidenhagen R, Gruetzner KU, Wiecken T, Spelsberg F, Jauch KW. Endoscopic vacuum-assisted closure of anastomotic leakage following anterior resection of the rectum: a new method. Surg Endosc. 2008 Aug;22(8):1818-25. doi: 10.1007/s00464-007-9706-x. Epub 2007 Dec 20. PMID: 18095024.
- Jimenez-Rodriguez RM, Araujo-Miguez A, Sobrino-Rodriguez S, Heller F, Díaz-Pavon JM, Bozada Garcia JM, De la Portilla F. A New Perspective on Vacuum-Assisted Closure for the Treatment of Anastomotic Leak Following Low Anterior Resection for Rectal Cancer, Is It Worthy? Surg Innov. 2018 Aug;25(4):350-356. doi: 10.1177/1553350618771410. Epub 2018 Apr 27. PMID: 29701133.
- Swedish Council on Health Technology Assessment. Vacuum Assisted Wound Closure Therapy [Internet]. Stockholm: Swedish Council on Health Technology Assessment (SBU); 2011 Nov 2. SBU Alert Report No. 2011-09. PMID: 26153601.
- Kühn F, Janisch F, Schwandner F, Gock M, Wedermann N, Witte M, Klar E, Schiffmann L. Comparison Between Endoscopic Vacuum Therapy and Conventional Treatment for Leakage After Rectal Resection. World J Surg. 2020 Apr;44(4):1277-1282. doi: 10.1007/s00268-019-05349-5. PMID: 31965274.
- Mees ST, Palmes D, Mennigen R, Senninger N, Haier J, Bruewer M. Endo-vacuum assisted closure treatment for rectal anastomotic insufficiency. Dis Colon Rectum. 2008 Apr;51(4):404-10. doi: 10.1007/s10350-007-9141-z. Epub 2008 Jan 15. PMID: 18197452.