Review Article
Utilizing Pulsed Electromagnetic Field (PEMF) Therapy (Diapulse®) for Drug-Free Pain Management to Eliminate Reliance on Opioids for Non-Malignant Chronic Pain: A literature Review and Proposal for Pilot Study

Thomas A Sharon*
Clinical Nurse Practitioner, Touro University Nevada, Nevada, USA
*Address for Correspondence: Thomas A Sharon, DNP, MPH, ARNP-BC, Clinical Nurse Practitioner at Touro University Nevada, Nevada, USA, Tel: (305) 917-3032; Email: [email protected]
Dates: Submitted: 07 September 2018; Approved: 14 June 2019; Published: 17 June 2019
How to cite this article: JSharon TA. Utilizing Pulsed Electromagnetic Field (PEMF) Therapy (Diapulse®) for Drug-Free Pain Management to Eliminate Reliance on Opioids for Non-Malignant Chronic Pain: A literature Review and Proposal for Pilot Study. Clin J Nurs Care Pract. 2019; 3: 027-34. DOI: 10.29328/journal.cjncp.1001013
Copyright License: © 2019 Sharon TA. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
The Federal and State governments have declared the presence of an opioid addiction pandemic in the United States claiming the lives of more than 55,000 in 2015 (Rudd RA, Seth P, David F and Scholl L. 2016). The pharmaceutical manufacturers of the numerous FDA-approved opioid drugs are raking in more than $5 billion per year with about 2 million chronic pain sufferers addicted. The irony of this narcotic use and abuse conundrum is the existence of evidence-based technology for drug-free pain management which is not covered for reimbursement among public and private third-party payers. Therefore, this paper is presented to propose a pilot study to demonstrate the efficacy of resolving the chronic inflammation, edema and ischemia that causes non-malignant chronic pain with PEMF therapy, a non-invasive, non-thermal radio transmission of electrical impulses, thereby invalidating the legitimacy of prescribing opioid analgesics in such cases.
Literature Review
Identifying the problem – the opioid addiction pandemic and the pain management fiasco
The fast-track proliferation of opioids in the United States began in the 1990s when pain became the fifth vital sign for hospitalized post-surgical patients, while a new consensus had developed declaring chronic pain to be a disease [1]. Van lee [2] exemplified Purdue Pharma’s aggressive promotion and marketing of Oxycontin (an extended release form of Oxycodone) as an illustration of large scale addiction and death being the consequence of profit motivation. Purdue Pharmaceutical’s sales of Oxycontin grew from $48 million to $1.1 billion from 1996 to 2000. The author attributed this exponential growth to 5,000 physicians being recruited for the Purdue Pharmaceutical’s speakers’ bureau at all-expense paid resorts and enticed the with lucrative speaking engagement fees. These physicians in turn promoted Oxycontin to the physician community-at-large for cancer-related and chronic low back pain. Purdue Pharmaceutical’s locked in their market share of opioid sales by offering the first 7-30 days’ supply for free while lying about the negligible risk of addiction. As expected, once the consumers became physically dependent, future sales were assured; the same nefarious scheme drug dealers employ to hook their customers. In 2007, the parent company, Purdue Frederick and three executives pled guilty to criminal charges of lying to the consuming public about the expected rate of addiction. However, by 2004, the damage was wide spread and irreversible with Oxycontin leading the pack in diversion and abuse.
The Centers for Disease Control and Prevention (CDCP) reported a nearly 300% increase in opioid overdose deaths from 1999 to 2014 [3]. The CDCP also reported 63% of the 52,404drug overdose deaths were attributable to opioids identified as “natural/semisynthetic opioids, methadone, heroin, and synthetic opioids other than methadone (P. 1445).” The opioid overdose death rate had increased from 12.3 per 100,000 population to 16.3 between 2010 and 2015. Additionally, the death from overdose of synthetic opioids increased 72% from 2014 to 2015 compared to the Heroine death rate increase of 20.6%. The CDCP recommended expanding prescription monitoring programs, implementing new guidelines for opioid prescribing, expanding Naloxone distribution and reducing illicit opioid supply. In short, the “experts” at the CDCP recommended rehabilitating the pharmaceutical industry’s opioid proliferation mechanisms with easier access to the overdose antidote, i.e. the opioid antagonist, Naloxone. Thus, the CDCP has set goals for the mere curtailment of the opioid addiction pandemic but offered nothing for its resolution.
Lyapustina and Alexander [1], attributed the current opioid addiction pandemic to aggressive pharmaceutical marketing of Oxycodone for non-malignant pain and inappropriate prescribing. These authors cited the lack of consensus among prescribers regarding appropriate dosing levels and source of pain to be treated with opioids as root causes for the massive numbers of addicted patients. They impugned the large-scale diversion of opioids from legitimate to illicit use as the reason for the large scale opioid related deaths suggesting the origin of all abuse of pharmaceutical opioids is provider prescription. The attempted solutions currently in place are mostly prescription surveillance conducted by third party payers, pharmacies and state regulators who provide pharmacy-generated controlled substance consumption records online. However, according to Lyapustina and Alexander the outcome of such surveillance efforts in rolling back or at least stunting the growth of opioid proliferation and death is yet undetermined. Moreover, these authors astutely articulated the continued failure of pain management in the United States notwithstanding that Americans’ consumption of morphine, Oxycodone, and Hydromorphone exceeds that of all other nations combined. There is no mention of any evidence-based drug-free pain management modalities which have been available and marginalized by stakeholders for decades.
Gostin, Hodge and Noe [4] offered evidence to bolster President Trump’s declaration of the opioid epidemic as a national emergency, the social implications of which empowers public health officials to take unilateral actions, marshal untapped resources and enable ground-breaking public health approaches. Two million (10%) of the 20 million substance abusers 12 years of age and older in the United States are addicted to prescription opioid analgesics. Pain management, promoted as a vital component of medical care since the 1990s has become a colossal failure with opioid analgesics as the primary treatment for long-term pain relief because of tolerance requiring large and larger doses to achieve the same effect. The unintended consequence of this fiasco is the 156% increase in the opioid overdose national yearly death toll from 2010 to 2015 starting with 21,088 and ending with 33,091 according to these authors. They also point out that the national emergency declaration will likely bring about draconian interventions by law enforcement to limit consumer access to opioids without addressing the efficacy of pain management and once the death tolls return to lower levels, with massive numbers of people experiencing withdrawal symptoms, this emergency intervention will likely end. What’s missing from this national emergency discussion is a redirection of pain relieving efforts to move away from opioids and toward evidence-based non-pharmacological pain relief, such as PEMF therapy.
The evidentiary basis for utilizing PEMF therapy to reduce non-malignant pain without opioids
In view of the foregoing, the PICOt question that provided the foundation for a literature review of the evidence was, “Does the application of pulsed electromagnetic field energy (PEMF) aka “pulsed radio frequency energy” (PRFE) (I) reduce or resolve non-malignant chronic pain through angiogenesis, edema resolution and anti-inflammatory effect (O) in people with chronic inflammatory diseases, traumatic tissue damage, peripheral nerve damage and/or chronic ischemia (P) as measured with cytokine blood levels, laser Doppler scanning for level of blood perfusion, daily doses of milligrams of morphine equivalent, pain intensity levels, and functionality indices?” Using the PICOt question key words for a literature search, two medical databases (Pub Med and Google Scholar) were explored for the best evidence on the use of PEMF for improvement of peripheral blood perfusion, reduction of inflammation and edema, reduction of daily opioid doses with a concomitant reduction of pain intensity levels and improvements in functionality as a basis for this proposal.
Guo, Kubat, Nelson and Isenberg (2012) performed a meta-analysis on 186 clinical studies published in the literature reporting consistently successful outcomes from using PEMF therapy in three clinical applications: 1) Postoperative (PO) edema and pain; 2) Non-postoperative (NPO) edema and pain; 3) Wound healing (WH). The reviewers grouped the 186 studies into the three basic categories and constructed a matrix to be able to match comparable data points across the various studies for the statistical meta-analysis. The 186 case-control studies under review were published over two decades in different parts of the world by non-related research teams and produced consistent results showing clinical efficacy in higher doses and non-efficacy in low dose therapies. This meta-analysis demonstrated that there was statistically significant evidence of wound healing and pain reduction efficacy in a clear majority of the 186 studies under consideration. The authors concluded PEMF therapy in sufficient doses is clinically effective in wound healing and pain management of traumatic soft tissue damage and chronic disease.
Harper, Schmidt, Kubat, and Isenberg [5] conducted an open label pilot study of PEMF therapy for failed back surgery pain. The authors defined failed back surgery syndrome as chronic back pain (often radiating to one or both legs) after spinal surgery. The percentages of spine surgeries that end with chronic intractable pain range from 19 % to 46% depending on the specific procedure. These authors noted, given the high volume of such surgeries, the inability of the medical community to effectively manage such pain has enhanced the rapidly growing opioid-addicted subculture of post-operative patients. To address the aforesaid problem, these authors conducted an open-label, single-arm pilot study to evaluate the analgesic effectiveness of PEMF. They included 4 to 13 subjects at each of four treatment sites. The subjects were provided with a portable PEMF device used at home which they applied twice per day for 45 days. In a post-treatment ad hoc survey, responders stated 44% and55% reduction in respective back and leg pain levels on average. Half of the responders showed reductions in opioid consumption in their medication consumption diaries issued at the beginning of the study. Sixty-seven percent of subjects who completed the study (86% compliance rate) expressed improvement in their overall well-being.
Reddy [6] examined the effectiveness PEMF therapy in reducing pain in participants with lateral epicondylitis (tennis elbow). The study group consisted of 22 subjects diagnosed with condition under review. Each of the subjects was treated 5 times per week for six weeks totaling 30 treatments. The pain was measured with visual analog pain scales. A pressure algometer was used to measure pressure-pain threshold in kg/cc. A handheld dynamometer was used to measure pain free grip strength in kg. All the treated subjects improved following 6 weeks of PEMF therapy. The mean pain score dropped from 7.82 to 3.11, PPT mean increased from 2.95 kg/cc to 4.84 kg/cc, and painless grip strength mean was enhanced from 18.6 kg to 22.1 kg. All the results were statically significant (P<0 .001) using a before vs. after T-test comparison. The author concluded PEMF treatment was effective in decreasing pain and improving function in patients with lateral epicondylitis.
Rohde, Taylor, Alonso, et al. [7], conducted a double-blind, placebo versus treatment, randomized study with 32 patients who were post-operative for TRAM flap breast reconstruction. The study cohort was randomly divided into a treated group with active pulsed electromagnetic field therapy and a placebo control group with a sham device. Outcomes were measured with visual analogue scale, opioid dosages, wound exudate volume and levels of interleukin – 1β beginning 1 hour after surgery. The average pain scores were 50% less in the treated group after 5 hours and 75% less at 72 hours (P<0.01) when compared to the sham. The treated group simultaneously showed 50% less mean opioid dosages (P<0.01). Wound exudate volume was 100% higher in the sham cohort at 24 hours (P<0.01), and mean interleukin – 1β concentration in wound exudates of treated patients was 80% lower than the sham group at 24 hours (P<0.001). The authors concluded PEMF therapy significantly reduced postoperative pain, inflammation, and narcotic use following TRAM flap breast reconstruction.
Graak, Chaudhary, Bal, and Sandhu [8] compared the effect of PEMF versus conventional treatment in subjects with diabetic polyneuropathy. There were two PEMF-treated groups with ten subjects each receiving dosages at 600 and 800 Hz respectively applied to the calf muscles of both legs. The PEMF treatment was applied for 30 minutes for each leg per day for 12 consecutive days. The third group (10 subjects) served as control and received standard medical treatment. The researchers used standard electromyogram (EMG) to measure distal latency, amplitude and nerve conduction velocity of all participants pre and post treatment. There were statistically significant reductions in the pain level scores in groups 1 and 2 compared to the control: 66.6, 63.25, and 22.5%, respectively showing PEMF to be 300% more effective than conventional medicine. The motor nerve functionality in the treated groups also showed significant improvement versus the controls.
Bagnato, Miceli, Marino et al. [9], examined the effectiveness of a PEMF device in the management of pain in knee osteoarthritis patients with a randomized, double-blind, case-control trial. The 60 of 66 subjects remaining to completion all had knee osteoarthritis confirmed on X-ray with persistent pain higher than 40 mm on the visual analog scale (VAS). The subjects wore the PEMF devices for 12 hours daily for 30 days. The primary outcomes were measured via the change in mean VAS and WOMAC scores. Secondary outcomes measures were changes in the quality of life assessment through the 36-item Medical Outcomes Study Short-Form version 2 (SF-36 v2), pressure-pain threshold (PPT) and changes in NSAID and opioid consumption. The PEMF treatment induced a 73% reduction in mean VAS pain and 34% reduction in mean WOMAC scores versus the sham device. Additionally, there were improvements in pain tolerance and physical health in the treated group. 26% of participants in the PEMF group stopped their NSAID/opioid therapy. There were no untoward occurrences. The authors concluded PEMF therapy is effective for pain management in knee OA patients.
The mechanism of action of PEMF therapy
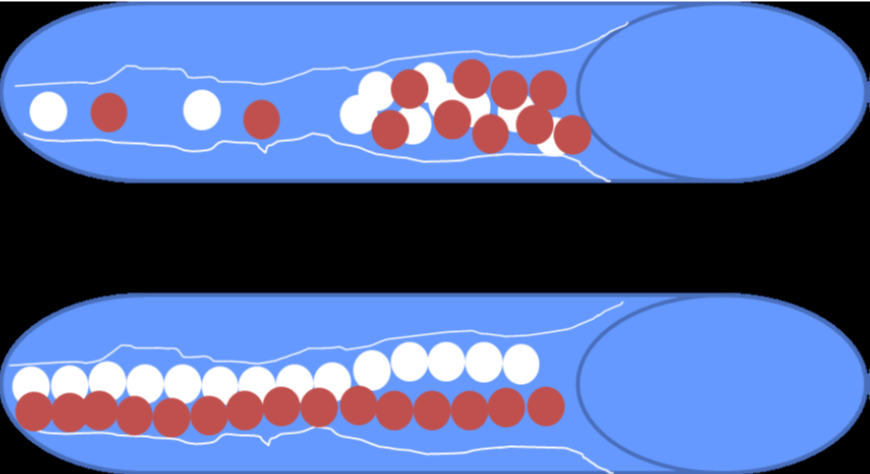
The mechanism of action when applying PEMF energy to the skin surface is still mostly theoretical. One long standing postulate on how PEMF improves the efficiency of microcirculation in ischemic tissue is the pearl chain effect theory on red and white blood cells introduced by Ginsberg (1958). Ginsberg observed the fat globules floating randomly in milk had formed pearl chains when exposed to Diapulse® PEMF due to magnetic polarization of each globule and returned to floating randomly a few minutes after the PEMF was turned off. Thus, the researcher proposed that PEMF initiates magnetic polarization of red and white blood cells adhering to like cells causing them to move through the vasculature in single-file, pearl chain-like formation rather than randomly floating about in the serum as illustrated below in figure 1. This alleged non-invasively induced physiological response may result in red and white blood cells moving more efficiently through the small arteries and arterioles with narrowed lumen without changing the hemodynamic, bringing more oxygen and nutrients to the peripheral tissue and removing waste, thereby allowing the body to begin the process of angiogenesis and nerve regeneration.
Costin, Birlea and Norris (2012) in conducting biochemical and physiological analyses in wounds undergoing PEMF therapy proposed three main effects: 1) an anti-inflammatory effect, by lowering the cytokine blood levels, thereby initiating the transition of chronic inflammation to an anti-inflammatory state; 2) a neo-angiogenic outcome, by increased endothelial cell propagation with tubulization and production of fibroblast growth factor (FGF-2); and 3) a re-epithelialization effect in open wounds through stimulation of collagen formation. Additionally, the finding of significant reductions of interleukin – 1β in post-operative wound exudate by Rohde, Taylor, Alonso, et al. (2015), corroborates the proposed anti-inflammatory properties of non-thermal PEMF energy.
Sharon [10] conducted a pilot study to investigate the effects of PEMF therapy on Plantar Skin Blood Perfusion in People with Diabetes Mellitus Type 2. The stated purpose of this study was to provide an evidentiary basis for using PEMF therapy in a primary care setting to promote microvascular angiogenesis, thereby achieving peripheral nerve regeneration to reverse the deleterious and painful effects of peripheral lower extremity neuropathy. This researcher treated 7 people between the ages of 54 and 65 with 10 to 22 daily PEMF therapy sessions of 30 minutes each. Each patient was tested with a digital laser Doppler device to measure red blood cell (RBC) concentration in the plantar skin of both feet. The foot with the poorer level of RBC perfusion was treated. Using the Wilcoxon signed rank test, there was a significant increase in volume concentration of moving RBCs (number of cells per second) and a concomitant decrease in RBC speed (P = 0.18 for both). The mean increase in RBC perfusion was 300%.
Methodology
Theoretical framework
The design of this proposed study was created in response to a dire need of the US population to reduce the inappropriate reliance on prescribed opioids to manage non-malignant chronic pain. The etiology of such pain encompasses a wide variety of underlying conditions from all types of traumatic tissue and nerve damage to a plethora of inflammatory diseases. Schneiderhan, Clauw and Schwenk [11] expressed concern over primary care providers not understanding the difference between acute and chronic pain, leading to chronic opioid use with inevitable tolerance and addiction. The change in medical paradigm during the 1990s re-categorizing chronic pain as a disease rather than a symptom of an underlying condition has caused conventional medical wisdom to evolve into conventional medical foolishness, sprinkled with corruption promulgated by big pharma executives behaving like drug cartel linchpins with impunity.
It is well known that non-malignant chronic pain can emanate from any area of the human body arising from some chronic inflammatory process that is either endogenous (autoimmune disorder or various types of injuries) or exogenous (pathogenic or foreign material invasion). The latter can be treated by attacking the pathogen or removing the foreign material while the former is more insidious with elusive resolutions and requires continuous management. Therefore, by approaching this pandemic health problem in treating such inflammation as a major underlying etiology of non-malignant chronic pain with a non-invasive modality such as drug-free PEMF therapy, we could make a substantial dent in reducing indiscriminate prescriptions for opioids and reducing its current level of consumption. To accomplish this goal there needs to be a paradigm shift from chronic pain management to chronic inflammation management.
Study design
The proposed study will require a cohort of 30 participants to be three times weekly for thirty minutes each with the Diapulse® PEMF therapy device. The cohort with be randomly selected from a patient population in Las Vegas, Nevada currently receiving opioids for pain management. This group will received thrice weekly 30-minute treatments with the Diapulse PEMF therapy device at maximum output of peak power at 6 and frequency at 600 on-off cycles per second.
The outcomes measurements will consist of standard visual analog system for pain intensity levels, pain tolerance levels, daily opioid dosage measured in morphine equivalence, a standard functionality index and cytokine blood levels. The investigators will compare the results of treatment to the stated parameters measured prior to commencing the PEMF treatments.
Hypotheses
The null hypothesis Ho: There will be no difference in outcome comparing pre and post treatment.
The alternative hypothesis H: The subjects will show a statistically significant reduction in pain and opioid consumption in the before and after comparison.
Sample selection
The 30 recruited subjects will be between 21 and 65 years of age with a diagnosis of chronic pain due to an inflammatory process excluding infection and/or presence of foreign material. The participants will also have been taking any amount of prescribed opioid(s) for a minimum of 30 days. The underlying diagnoses will include but not be limited to fibromyalgia, post laminectomy syndrome, failed back spine surgery syndrome, diabetic neuropathy, compression neuropathy, sciatica, post herpetic syndrome, radiculopathies at cervical, thoracic and/or lumbar levels, osteoarthritis, rheumatoid arthritis, psoriatic arthritis and multiple sclerosis. Each participant will undergo a urine drug screen prior to beginning the study and the presence of illicit drugs or non-prescribed controlled substances will be exclusionary.
Statistical model
The one-tailed T-test will be utilized to determine the statistical significance of the difference between the pre and post treatment measurements of the dependent variables listed as follows:
• Cytokine blood levels
• Pain intensity level
• Pain threshold level
• Amount of daily opioid consumption measured in Morphine equivalence
• Functionality index
The independent variables will be as follows:
• Demographics
• Diagnosis of chronic pain due to chronic inflammation
• Prescription opioid consumption for at least 30 days prior to start date
Materials and procedures
This proposed study which will be conducted at the offices of Mind Body Solutions. The investigator will begin with obtaining informed consent. The researcher will then conduct a history of present illness and brief physical exam. A phlebotomist will draw blood for a cytokine level. The research worker will then assist the participant in filling out the questionnaire to elicit pain intensity, pain threshold, amount of opioid consumption which will be confirmed on the Nevada State PMP website and urine drug screen. Finally, the participant will complete the questionnaire to determine the functionality index.
For the PEMF therapy, this investigator will use a Diapulse® Model D103 electromagnetic therapy device manufactured by the Diapulse Corporation of America. This device emits a pulsed electromagnetic field through a radio transmitter at a radio frequency of 27.7 MHz with peak power adjustable from 1-6 and pulse frequency adjustable from 80 to 600 cycles per second (cps). Each subject in this study will be treated with peak power set at 6 (975 Watts per pulse) and pulse frequency set at 600 cps, which the manufacturer’s suggested level for full anti-inflammatory effect. The Diapulse® device (Figure 2) has been FDA approved for treating pain and edema in soft tissue since 1986. In 2004, the Center for Medicare/Medicaid Services (CMS) established a designation of the Diapulse® device as electromagnetic therapy and authorized reimbursement for treating chronic wounds defined as wounds that do not respond to 30 days of conventional wound care therapy.
Proposed budget| Item | Unit Cost | Quantity | Total |
| Diapulse Model # D103 PEMF device purchase | $25,000 | 2 | $50,000 |
| Diapulse Model # D103 PEMF sham device purchase | $25,000 | 2 | $50,000 |
| Nurse Practitioner for three months | $32,500 | 1 | $32,500 |
| Research assistants for three months | 10,000 | 2 | $20,000 |
| Total budget | $152,000 |
Discussion
Since President Trump has declared the opioid addiction pandemic to be a national emergency, the Drug Enforcement Agency and State Pharmacy regulators across the country have mobilized in creating new laws and regulations to limit the number of opioid pills that can be prescribed at any given time. Pain management patients are being required to refill their prescriptions twice as often and the maximum allowable morphine equivalent dosage guideline is now at 90 mg. per day. The appropriateness of prescribing opioids for chronic non-malignant pain in primary care is now being called into question to some extent [11]. However, there are no solutions being offered to replace opioid consumption with a non-pharmacological non-invasive anti-inflammatory modality such as PEMF therapy. Pain management as a medical specialty has been a massive failure because the most common method of treatment is long term opioid consumption. The popular trend declaring pain to be a disease rather than a symptom since the 1990s has led to the large-scale masking of pain-causing chronic inflammation, leaving the underlying condition mainly untreated. Moreover, the universal side effect of opioids, called “tolerance,” requires larger and larger doses to achieve the same effect leaving patients at risk of dying from opioid-related complications.
References
- Lyapustina T, Alexander CG. The prescription opioid addiction and abuse epidemic: how it happened and what we can do about it. The Pharmaceutical Journal. 2015; 11: 1-9. Ref.: http://bit.ly/2X7YzFv
- Van Zee A. The Promotion and Marketing of OxyContin: Commercial Triumph, Public Health Tragedy. Am J Public Health. 2009; 99: 221-227. Ref.: http://bit.ly/2XFXWjn
- Rudd RA, Seth P, David F, Scholl L. Increases in Drug and Opioid-Involved Overdose Deaths — United States, 2010–2015. Morbidity and Mortality Weekly Report US Department of Health and Human Services/Centers for Disease Control and Prevention. 2016; 65: 1445-1452. Ref.: http://bit.ly/2XbCypc
- Gostin LO, Hodge JG, Noe SA. Reframing the Opioid Epidemic as a National Emergency. JAMA. 2007; 318: 1539-1540. Ref.: http://bit.ly/2KjaHxo
- Harper WL, Schmidt WK, Kubat NJ, Isenberg RA. An open-label pilot study of pulsed electromagnetic field therapy inthe treatment of failed back surgery syndrome pain. Int Med Case Rep J. 2015; 8: 13-22. Ref.: http://bit.ly/2RfxJ8L
- Reddy RS. Effect of pulsed electromagnetic field therapy on pain, pressure pain threshold, and pain-free grip strength in participants with lateral epicondylitis. Saudi J Sports Med. 2017; 7: 93-96. Ref.: http://bit.ly/2wVa30g
- Rohde CH, Taylor EM, Alonso A, Ascherman JA, Hardy KL. et al. Pulsed Electromagnetic Fields Reduce Postoperative Interleukin – 1β, Pain, and Inflammation: A Double-Blind, Placebo-Controlled Study in TRAM Flap Breast Reconstruction Patients. Plast Reconstr Surg. 2015; 135: 808e-817e. Ref.: http://bit.ly/2Zn8rsd
- Graak V, Chaudhary S, Bal BS, Sandhu JS. Evaluation of the efficacy of pulsed electromagnetic field in the management of patients with diabetic polyneuropathy. Int J Diabetes Dev Ctries. 2009; 29: 56-61. Ref.: http://bit.ly/2Xcs1tH
- Bagnato GL, Miceli G, Marino N, Sciortino D, Bagnato GF. Pulsed electromagnetic fields in knee osteoarthritis: adouble blind, placebo-controlled, randomized clinicaltrial. Rheumatology. Rheumatology (Oxford) 2015; 55: 755-762. Ref.: http://bit.ly/2Fbmj17
- Sharon TA. An Investigation of the Effects of Pulsed Electromagnetic Field Therapy on Plantar Skin Blood Perfusion in People with Diabetes Mellitus Type 2: A Pilot Study. 2015; 3732465. Ref.: http://bit.ly/2WHVmx1
- Schneiderhan J, Clauw D, Schwenk TL. Primary Care of Patients with Chronic Pain. JAMA. 2017; 317: 2367-2368. Ref.: http://bit.ly/2IfsrHF